
This information is for people with multiple sclerosis (MS) aged 65 and older. It’s also useful to people under 65 who are thinking about their future years, as well as friends, family and caregivers of people with MS.
Here, you can learn about the positive steps you can take to protect your health, wellbeing and independence as you get older. Each section has tips on ways to actively manage your health and wellbeing.
We hope this information supports you in having a positive experience of getting older with MS and reduces any fears about the future.
We would like to thank the Multiple Sclerosis International Federation (MSIF) for their permission to adapt this resource. The original MSIF resource Living well with MS as you grow older can be viewed here on the MSIF website.
Check out our Hear From the Experts webinar all about Aging and MS
Why Focus on MS at an Older Age?
We’re seeing more older adults living with MS, with the highest number of people living with the disease now between 55 to 65 years old. Living well with MS at an older age means managing both MS and age-related health issues.
As we get older our bodies change, which can bring new challenges for living with MS. We also become more likely to develop additional health conditions.
MS symptoms tend to progress over the years. As they get older, people with relapsing-remitting MS will have fewer periods where their symptoms come and go. The disease usually becomes secondary progressive MS over time, meaning that symptoms steadily worsen.
For these reasons and more, people with MS are more interested in how they can maximize their physical and cognitive abilities, manage their MS well, and get the most out of life as they get older. This is sometimes called ‘healthy aging’.
The good news is that getting older can bring the experience and wisdom to better manage MS.
In a study, many older adults with MS said they had gained confidence in managing their disease and had a better quality of life now than before. In another study, people with MS in their 80s reported less fatigue and stress than those in their 60s.
However, older people with MS face some increasing challenges. For example, people over 65 years old with MS report challenges with things like bathing, dressing and getting around the house or community. Common concerns included:
-
being less mobile
-
becoming a burden to family and friends
-
requiring more care.
What general approaches help people to live well with MS as they age? Connecting with others, attitude, lifestyle choices and healthcare have all been reported as important, as you can see in the graphic below.
It’s encouraging that most of the themes people found helpful are things we can change. You’ll see these themes appear often in this resource.
Based on a survey of almost 700 Canadians aged 55 or older
1
Social Connections
Including:
- Friends and family
- Communities and groups
- Caregivers
3
Lifestyle choices and habits
Including:
- Healthy diet and exercise
- Managing medicines
- Self-care and rest
2
Attitude and outlook on life
Including:
- Positive thinking
- Being determined and persevering
- Accepting limitations
4
Health Care
Including:
- Being able to get high quality care
- Good relationships with healthcare providers
- Being heard
Additional factors some people find important are:
Spirituality and religion
Independence
Finances

How Age MS and Other Conditions can Affect Your Health
As you get older, your body and brain health will change. Some of these changes may overlap with your MS symptoms. You might also get symptoms from other health conditions.
In this section, we look at:
overlapping symptoms of getting older and MS
common health conditions in older people
how other conditions might affect your MS and treatment options
As we get older, our bodies change in many ways. For example, our muscles become weaker, we may tire more easily, our cognitive abilities (thinking, learning and memory) can decline, bladder control can weaken, and vision can change. If you have MS, some of these changes may sound familiar because the disease can affect these aspects of your health too.
This overlap can make it hard to know whether problems you’re experiencing are related to your MS, are signs of growing older or both.
|
|
Older age |
MS |
|---|---|---|
|
Energy levels |
Tiring more easily |
Fatigue |
|
Movement |
Reduced muscle tone, strength, and flexibility, slower movement, an increased risk of falls |
Reduced mobility, strength, coordination and balance, an increased risk of falls, speech difficulties |
Bladder |
Greater urgency and frequency of urination, reduced bladder control, more frequent infections |
Greater urgency and frequency of urination, reduced bladder control, more frequent infections |
|
Digestive system |
Less appetite, indigestion, constipation |
Constipation |
Sex |
Altered sex drive or enjoyment, vaginal dryness, difficulty keeping an erection |
Altered sex drive or enjoyment, vaginal dryness, difficulty keeping an erection |
|
Vision |
Poorer near vision, reduced night vision |
Blurred or double vision, blind spots, jerky vision |
Cognitive function |
Slower to process information, reduced attention, reasoning, and memory |
Slower to process information, reduced attention, learning, memory, and reasoning |
Mental health |
Depression | Low self-esteem, depression, anxiety, mood swings |
Bones and joints | Weaker bones, stiffer joints | Weaker bones |
As you get older, you’re more likely to develop other health issues alongside your MS. These are also called comorbidities. Some comorbidities are more common in people living with MS than in the general population. These include depression, anxiety, diabetes and high blood pressure.
About 5–6 in every 10 people over 60 with MS have high blood pressure. More than 2 in every 10 have high levels of lipids (fats such as cholesterol) in the blood, and a similar proportion have a chronic (long-term) lung disease. Some health conditions become more likely as we get older (see graphic).
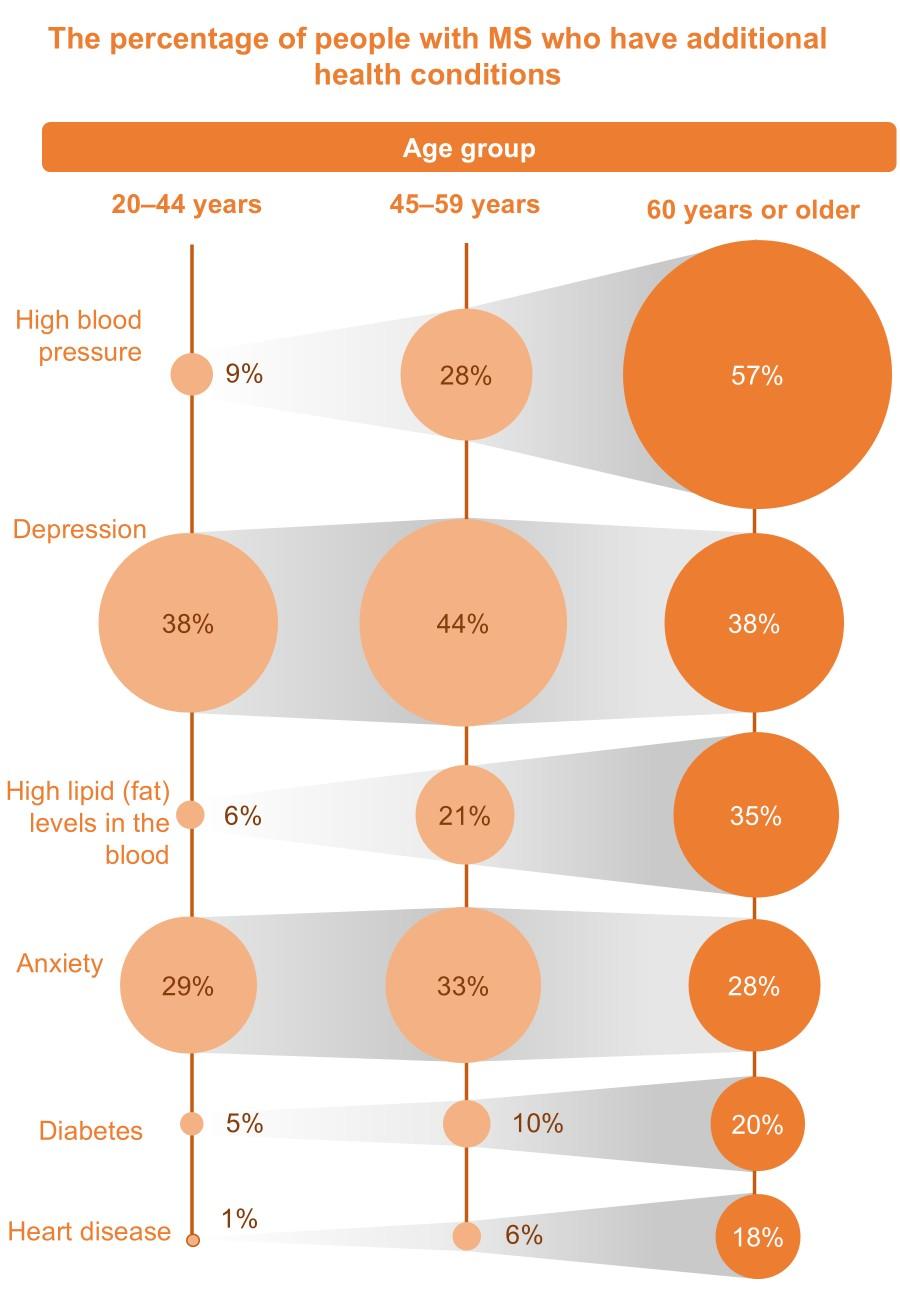
| 20-44 years | 45-59 years | 60 years or older | |
|---|---|---|---|
| High blood pressure | 9% | 28% | 57% |
| Depression | 38% | 44% | 38% |
| High lipid (fat) levels in the blood | 6% | 21% | 35% |
| Anxiety | 29% | 33% | 28% |
| Diabetes | 5% | 10% | 20% |
| Heart disease | 1% | 6% | 18% |
Graphic reproduced and adapted from ‘Why manage comorbidities in people with multiple sclerosis?’, with permission from Oxford Health Policy Forum. (https://www.msbrainhealth.org/healthcare-professionals/why-manage-comorbidities-in-people-with-multiple-sclerosis/)
Women may also experience problems during and after menopause. These can include bladder problems, changes to sex life, sleep problems and depression.
Read Menopause and MS for more information.
If you have another health condition, some of its symptoms may overlap with those of your MS. Your doctor can help to identify the cause of any new problems you experience. They can also give you advice on how to manage the two conditions together.
While you’re experienced at managing your MS, learning to manage new health needs can feel challenging. In a study, older people with MS said they were more concerned about their other health conditions than their MS.
Managing your other health conditions well is important. This will help to reduce any impact they might have on your MS, general health, cognitive abilities and quality of life.
Some health conditions may worsen or add to your MS symptoms, especially if they are not well controlled. For example, studies suggest:
-
People who have a cardiovascular condition at the time they’re diagnosed with MS are likely to need a cane to walk sooner than other people with MS.
-
People with MS who have higher levels of cholesterol (a type of fat) in their blood have more disability and more brain shrinkage than those with lower cholesterol levels.
-
People with MS who are depressed or anxious may not take their MS medicines as prescribed, or sometimes stop taking them altogether. This is important because if medications are not taken as prescribed, the disease may not be controlled properly.
Some health conditions don’t affect MS directly. However, they may add further challenges to your everyday life.
Treatments are available to manage MS, known as disease-modifying therapies (DMTs). If you have certain other health conditions, some MS treatments might be less suitable for you. This can be for a variety of reasons, including:
-
Certain medical conditions increase the risk of an MS treatment causing serious side effects. For example, if you have cardiovascular problems (like a recent heart attack or stroke) or are taking beta-blockers or calcium channel blockers for high blood pressure, some MS treatments will not be suitable for you. Your doctor will be able to explain which treatments are suitable for you, and why.
-
Some treatments for MS can affect the way other medications act in your body, and vice versa. This is known as a drug–drug interaction. For example, some MS treatments can affect how quickly your body processes other types of medications you may be taking. This might mean that the dose, the medications, or both should be reviewed.
-
If you regularly take five or more medications for MS and other health conditions, it’s important to work closely with your pharmacist or prescribing physicians. Reviewing your medications with healthcare providers helps prevent potential side effects and interactions.
Steps to Managing Your Health
To live well with MS as you get older, you’ll need to stay on top of your overall health and wellbeing.
In this section, we look at four simple steps you can take to manage your health:
1 Be alert to and report new symptoms to your doctor.
2 Have screening tests for other health conditions.
3 Diligently follow health advice.
4 Keep physically active.
New symptoms could be related to MS or your age. They could also be a sign of a new health problem.
If you have any new symptoms, share them with your doctor. By finding the exact cause, health professionals can give you the right treatment and advice. For example, fatigue caused by a sleep disorder or thyroid disease might be treated differently from fatigue caused by MS.
Sometimes, multiple things may contribute to your symptoms. You might need to see a few different healthcare professionals before they can work out the causes and determine the best treatments for you.
Your primary care provider is best placed to help with health changes due to age, while your neurologist can help you manage your MS. They may refer you to other specialists to help you manage other conditions.
For more information, check out our MS symptoms page.
As well as looking after your current health, consider having any screening tests you’re offered. Screening tests check for risks or warning signs of other conditions. Spotting these early means you can take steps to reduce your risk or manage a condition at an earlier stage. Depending on your local health authority, age and gender, screening available to you might include checks for bowel cancer, prostate cancer, diabetes, depression, cervical cancer, breast cancer and weak bones (osteoporosis).
Doctors, nurses and other health professionals can provide regular checks, advice, treatments and support. However, only you are in the position to protect your health and wellbeing every day. So, save some time and energy each day to devote to your health.
It can be hard to stay focused and follow health advice every day. However, some age-related changes and other health conditions may add to your health problems. Unhealthy habits like smoking can also worsen MS.
For everyone with MS, being more physically active can improve walking and physical function. Being regularly active may have additional benefits including:
-
better cognitive function
-
reduced MS symptoms
-
slower disease progression
-
help with depression
-
improved cardiovascular fitness
Whatever your age and fitness level, there are ways to keep active. You’ll need to find the right type of activity and intensity for you. Check with your doctor before starting a new physical activity plan.
You may need to be at least moderately active to get the benefits listed above. Examples of moderate activity are faster walking, gardening, swimming and cycling.
Some types of physical activity — including strengthening exercises, posture work and stretches — are possible seated.
Succeeding in being regularly physically active is about mindset as well as strength and stamina. You’re more likely to keep physically active if you set yourself goals and have confidence in your ability to achieve them.
Ways to ensure success include:
-
find activities you enjoy
-
make plans with others to exercise together
-
use an app to track your activity
-
join local physical activity groups
-
speak to your doctor or nurse about services to help you
Tips: Looking after your health and wellbeing |
|
Note down changes to your physical and mental health in a diary or app so you can discuss them with your doctor or nurse. |
Be open to hearing from friends, family and carers if they notice a gradual change in your health that you might have overlooked. |
Have a set routine for taking medications. A pill box, calendar or reminders on your smartphone may help. |
If you’re struggling to stay motivated or to fit your health needs into your daily life, ask your doctor or nurse what programmes or specialist support is available to you. |
Take up invitations for health screening. If you’re unsure what’s available, contact your family doctor’s clinic or insurer to ask. |
Taking control of your Health
Self-management is a set of approaches to manage (and improve) your physical health, mental health and wellbeing within your overall life. It can help you to:
- feel confident and positive about managing your MS
- feel in control of your life and future
- cope with your MS symptoms
- improve your quality of life
Self-management is a valuable skill and can be very rewarding. It involves managing various aspects of your life to help you meet your goals. You can tailor approaches to match your personality, qualities, experiences, abilities and desires. We give a summary of what good self-management looks like in the graphic below.
What does good self-management look like?

Know their body well. They have knowledge of MS and how it affects them physically and mentally.
Lead a healthy lifestyle, including a good diet and regular exercise and relaxation.
Have established routines to manage their MS that work well for them. They adapt these when needed.
Have a strong sense of their roles in family and society. They have forged a life that is rewarding and brings enjoyment.
Spot changes to their physical and mental health, sleep patterns, energy levels, eating and mood. They then can take action.
Are familiar with their emotions. They have techniques to turn around negative emotions like feeling frustrated or helpless.
Many people with MS feel they’ve become better at managing their disease and symptoms as they’ve gotten older.
In studies of living well with MS at older ages, some people explained that it took them almost 10 years to understand their MS. Once confident in how to predict and manage their MS symptoms, they were able to cope better and focus on the parts of their lives that were important to them.
Several wished they could have learned about their MS and gained that confidence earlier.
Generally, people who are living well with MS in older age are adaptable in their mindset.
In one study, many people felt that their ability to live well with MS as they got older was due to:
-
gaining wisdom
-
creating meaningful activities and relationships
-
being able to deal with their changing capabilities
Another study found that individuals with MS reported that, over time, their disease felt more predictable. They got used to their symptoms and how their bodies functioned with MS. Critical to their quality of life were:
-
socializing
-
access to healthcare
-
healthy lifestyle habits
-
being independent at home
On average, women with MS might be better able to adapt to growing older than men. Older men with MS can feel less resilient, might participate in things less, and can view their health as poorer. These are all things that self-management can help you to improve.
The ingredients of successful self-management can be broken down into six skills.
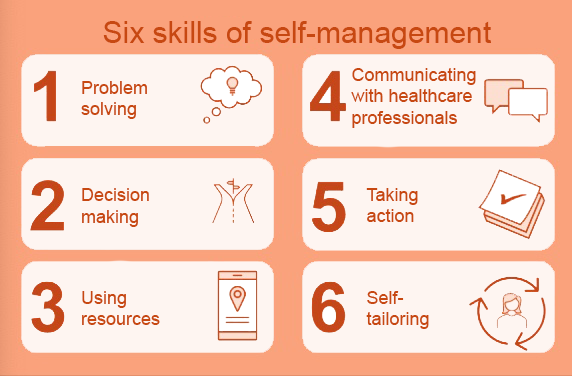
1. Problem solving
To problem solve, you first need to recognize and understand the problem. You can then work out possible ways to solve it and choose the best solution. For example, you may find that standing and cooking meals is too tiring. To problem solve, you could identify ways to reduce the time you spend cooking. You could then try out these different ideas, like making enough food for two meals, trying simpler recipes, or eating out on certain days of the week.
2. Decision making
Decision making can involve working out what is most important to you and deciding how to manage your daily activities. When faced with a busy day that might be too fatiguing, you could list the activities in order of priority. What do you most want to do? What must be done today? Can you postpone activities that are lower priority? For example, you might prioritize having coffee with a friend and doing some strengthening exercises but delay a trip to choose home furnishings.
3. Using resources
Resources are anything you use to help you complete a task, like technology, transport, the help of others, or a strategy. You also have your own resources, like your time and energy.
Good self-management involves organising yourself efficiently using the resources you have available. For example:
- You could group chores together to save time and energy. An example would be to combine exercise and grocery shopping by walking to the store and getting a bus back.
- You could set up online banking so you can avoid some trips to the bank.
4. Communicating with healthcare providers
Working in partnership with healthcare providers is an important part of self-management. Most people find that it is more helpful to have a two-way conversation with their healthcare providers rather than just being told what to do. One way to take ownership of your health is to prepare for healthcare visits by noting issues in a journal. Also write down discussions and outcomes. Share what’s important to you and your goals.
5. Take action
Often, taking planned action is the most difficult step in self-management. You might say ‘I intend to eat better’ but this is not an action. Developing new habits is the tricky part! By following your new plan often and consistently, you’ll find it will soon become the norm. For example, to improve your diet you could write down your goals, plan meals for the week, and then keep track of your progress.
6. Self-tailoring
Self-tailoring means modifying the things around you to suit your own needs and the resources you have available. Using this skill, you can find ways to make your health needs fit into your schedule. For example, if commitments (like work or childcare) mean that you’re not getting enough sleep, you could build rest periods into your day to catch up when it’s convenient. It’s a good idea to check any changes with your healthcare team.
Self-management is a continual learning process. To live well with MS as you get older, you’ll need to find ways to manage varying symptoms and challenges. By adapting your routines, you can reduce the impact of your MS and do the everyday things that matter to you.
Sometimes, changes in your life or health mean that an approach that worked well before no longer does. You might begin to feel weighed down by the demands of living with MS or the routines you put in place. Learning new approaches to self-management or changing tactics can help.
Developing positive and useful ways of thinking can help you to succeed in self-management. As you start to feel the benefits of self-management, this can make you feel more positive and confident too.
People who are good at self-management reflect on their own thoughts and feelings often.
Ask yourself:
-
How are you feeling physically and emotionally?
-
What are your strengths and are you making the most of them?
-
Do you have a plan of action and are you following it?
-
Do you need help, and who can provide it?
Of course, none of us feel positive all of the time. It’s normal to have times when it’s harder to see a way forward or to motivate oneself. Here are some feelings you might experience from time to time, along with ways to get back on track.
| What it looks like | What to do about it |
|---|---|---|
Denial |
|
|
Self-defeating thoughts |
|
|
Worrying |
|
|
Although self-management is about taking charge of your own health and life, this doesn’t mean you have to manage things alone. Making good use of the help and resources available to you is a fundamental part of self-management. Take some time to work out what help healthcare professionals, friends, family or caregivers can give you. Be willing to accept help when it’s offered.
Share your experiences and goals with others so they can support you. Connecting with your local, national and international MS communities can be extremely valuable. Through these, you can learn from others and share your own experiences.
Your Independence and Identity
Loss of independence is a common concern for people with MS as they get older. Losing some independence can also affect your sense of identity (how you feel that others perceive you) and sense of self (the person you feel you are).
In this section, we look at:
- the help you might need as you get older
- who might provide that help
- protecting your identity and boosting your self-esteem
Compared with younger people, those with MS who are over 65 years old say they have more difficulty with:
-
bathing, dressing and going to the toilet
-
getting out of bed or around a room
-
taking medication
-
shopping and getting around the community

Many people with MS do not progress to the point of serious disability. However, the effects of MS and getting older may mean you need to consider some adjustments to your lifestyle and level of independence.
You might need help due to physical limitations or changes in your cognitive function (thinking, learning and memory).
Help and support from a partner, family member or friend is invaluable to many older people with MS. Many older people with MS have help from professional caregivers too, which might be funded personally, publicly, through insurance, or a mix of these. People living alone are more likely to use professional help.
It’s natural to want to keep your independence. Becoming more dependent on others can feel like a threat to your freedom to do the things you want to do, and when. It can also make you feel vulnerable. However, accepting help will mean you can get more from life, not less.
People living alone or away from friends and family may worry about getting enough support. Conversely, it’s common for those living with a partner, friends or family to worry about being a burden.
If you currently provide care to others – such as older relatives or grandchildren – needing to take a step back can have practical and emotional impacts. Changing your roles in the family might alter your sense of identity or self, which we discuss below.
Receiving care from a partner, friend or family member can change both of your lives in many ways. It can also change the dynamics of your relationship. To keep your relationship healthy, talk openly about how you’re both feeling and your needs.
Changes you make to your life as you adapt to growing older can alter how you view yourself, including:
-
how you feel others perceive you (your sense of identity)
-
the person you feel you are (your sense of self)
-
how valuable you feel (your self-esteem).
This could affect your mood and mental health. Find activities, roles and friendships that support you in knowing who you are.
It can help to connect with others through groups or family. Organizations supporting people of older ages can also be a great source of practical and emotional support. Many provide advice and tips on dealing with big changes in later life such as retirement, becoming a grandparent, losing a loved one, or changes to independence. To work through your feelings, you might find a therapist’s help useful. If loss of identity or low self-esteem is affecting your mental health, speak to your doctor or a mental health professional.
Tips: Protecting your independence and identity |
Plan ahead. |
Research professional care services. |
|
Adapt your home. |
Use assistive devices. |
Connect with others. |
|
Do things that bring you joy. |
|
Work on relationships with caregivers. |
Your Cognitive Health
MS and growing older can both affect your brain health. This is the way your brain cells grow, change, function and recover. Brain health can affect your cognitive function (thinking, learning and memory), emotions, mental health, behaviour and some body functions.
In this section, we look at cognitive health including:
- how it can be affected by age and MS
- how cognitive difficulties might impact your daily life
- whether you can prevent or slow cognitive decline
- tips for improving your cognitive health
Just like a computer, your brain takes in information, stores it, processes it, and makes outputs. This is your cognition.
Many people – both with and without MS – experience some changes in their cognitive abilities as they get older. In one survey, more than half of people with MS aged 45–88 years old said they had cognitive difficulties that interfered somewhat with their daily lives.
Common effects of age and MS on cognitive function
The more common cognitive changes in older people with MS are:
-
taking longer to process information
-
reduced attention
-
learning and memory problems
Some older people with MS have reduced ‘executive function’. Executive function is more complex thinking. We use it to make and adapt plans and control our behaviour or emotions.
Your cognitive changes may be more noticeable when you’re tired or fatigued. This is temporary and should improve once you’re better rested. Emotions, anxiety, depression, MS relapses and medicines can also affect cognition.
Cognitive difficulties might affect your ability to do some daily tasks, hobbies or aspects of your job. We give some examples in the table.
Cognitive difficulties are often ‘hidden symptoms’ because they are not immediately obvious to others. Family or friends might find them hard to understand and cope with at times. This might affect your interactions with others and make you feel isolated.
Examples of how cognitive changes can affect your daily life
Taking longer to process information |
| |
|---|---|---|
Reduced attention |
| |
Learning and memory problems |
| |
Reduced executive function |
|
The effects of MS and age on cognition differ from person to person. MS can begin to affect cognitive function early in the disease process. In general, people with MS experience a fairly slow decline in cognitive function as they get older.
Having a well-stimulated brain might help to slow or lessen the impact of age and MS on your brain. It’s unlikely that you can avoid cognitive changes altogether. However, you might be able to reduce their impact on your daily life.
You can improve your cognitive ability with activities that:
-
engage your mind
-
make you curious
-
spark your creativity
-
get you thinking
-
challenge your problem-solving skills
Learning to adapt to cognitive changes can reduce their impact on your life. Physical activity has also been shown to improve cognitive health. Getting sufficient sleep and looking after your mental health can help too.
Tips: How to look after your cognitive health |
Stimulate your brain to improve your cognitive abilities.
|
|
Join a club or group. |
Get enough rest and sleep. |
Look after your mental health. |
Have checks on your cognitive abilities. |
Set up routines that aid your memory. |
Your Mental Health
When living with a long-term disease like MS, good mental health can make all the difference to your quality of life. On the other hand, poor mental health can make it harder to live with MS and prevent you from living your life fully. For example, depression can make it harder to stay active, eat well and connect with others.
You might feel confident in noticing and addressing mental health problems, or you might feel there’s a stigma attached to this. Views on mental health have changed greatly over the years. Younger generations are more aware of their mental health and open to finding support.
We would like to support older persons with MS in feeling able to discuss and care for their mental health, and we hope this information helps.
In this section, we look at:
how MS and age can affect mental health
how depression and anxiety can be treated
how to recognize mental health changes
the mental health of caregivers
tips on caring for your mental health
Living with MS can sometimes make you feel down, emotional or irritable. It can also affect your self-esteem. As we learnt in the last section, MS can also affect your brain health, which can have an emotional impact.
When issues like feeling down or anxious go on for a long time, or start to affect your everyday life, they are classed as a mental health condition.
Mental health conditions are common in people with MS. About half of all people with MS will get depression in their lifetime. This is a higher rate than seen in the general population. Suicidal feelings are also higher in people with MS than in the general population.
It’s possible to have more than one mental health condition; depression and anxiety often occur together in people with MS. It’s been found that in older people with MS, men are more likely to feel depressed, while women are more likely to be anxious.
We show some more facts in the graphic.
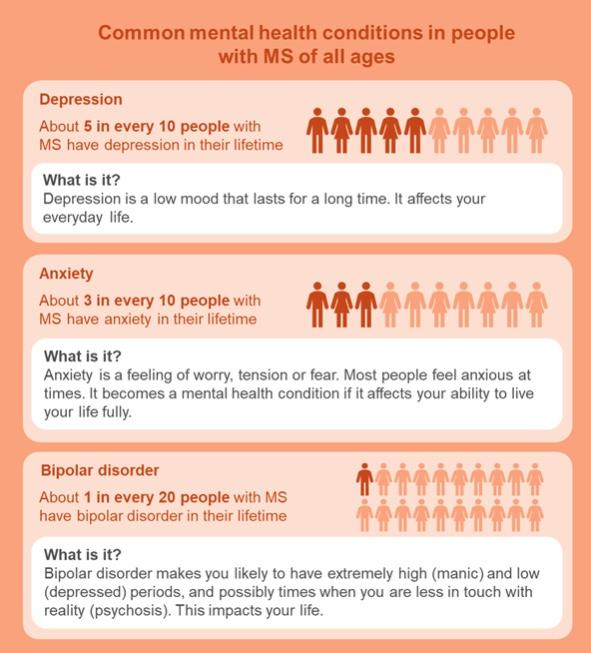
Depression
About 5 in every 10 people with MS have depression in their lifetime
What is it?
Depression is a low mood that lasts for a long time. It affects your everyday life.
Anxiety
About 3 in every 10 people with MS have anxiety in their lifetime
What is it?
Anxiety is a feeling of worry, tension, or fear. Most people feel anxious at times. It becomes a mental health condition if it affects your ability to live your life fully.
Bipolar disorder
About 1 in every 20 people with MS have bipolar disorder in their lifetime
What is it?
Bipolar disorder makes you likely to have extremely high (manic) and low (depressed) periods, and possibly times when you are less in touch with reality (psychosis). This impacts your life.
MS can affect your mental health in two main ways:
-
MS can affect your brain health. Structural or functional changes to your brain can make mental health problems more likely.
-
The symptoms of MS and their impact on your everyday life can affect your emotions, self-esteem and mental health.
Many people find they’re better able to cope with MS as they age. However, getting older with MS can sometimes affect mental health negatively.
Keep social connections with family and friends and try to meet new people. Feeling lonely and isolated can sometimes lead to depression and anxiety.
It’s not clear whether the chance of being depressed increases or decreases as people with MS get older. Some studies found that older people with MS were less likely to be depressed than younger people with the disease. Other studies found the opposite.
The chance of becoming depressed will be different from person to person and change throughout life. It may be affected by:
-
the level of MS disability you have
-
how well you cope with challenges
Your risk of depression can be affected by factors unrelated to your MS too.
You may feel there’s a logical explanation for feeling down or worried. After all, MS can impact your daily life in many ways and bring uncertainties about the future.
This does not mean that depression and anxiety are things you should ‘learn to live with’. You can treat them, and this can improve your life.
Depression and anxiety can worsen other symptoms of MS, like fatigue, pain, sleep problems and cognitive function. This is another reason to take action.
Depression and anxiety can be helped through:
-
talking therapies, which involve talking to a trained professional about your thoughts, feelings or behaviours
-
self-help programmes to learn to adapt your thinking patterns
-
medicines
Being physically active can also boost your mood and help with depression.
Depression is not always recognized in older people with MS, especially men. Be alert for the signs. Some of these are shown below.

Some people with depression get physical symptoms too, like pain, fatigue, or stomach-ache. Anxiety can also bring on panic attacks that make you feel like you can’t breathe.
If you think you might have a mental health condition, speak to your healthcare team. They can refer you to someone who can help.
If talking to a professional is daunting, you might find it easier to talk to a friend, family member, neighbour, carer or a charity advisor in the first instance. Depending on the services available to you, you might be able to see a trained counsellor or get community support or workplace support.
At its most severe, depression can be life-threatening. If you feel you might attempt suicide, contact the emergency services or call 9-8-8: Suicide Crisis Helpline now. If you don’t feel able to do this yourself, ask someone to help you.
If you feel down or anxious, it can be tempting to withdraw from others. It can also be harder to find the courage to make new connections. However, socializing is important for your mental wellbeing.
Older people affected by MS say that socializing is important to their quality of life.
Friendships and family relationships can bring you joy and prevent loneliness. Social connections can also be a source of empathy and support when you need it.
Try to have regular good-quality time with your loved ones. Be proactive about keeping in touch – even a brief phone call can make all the difference. Look for opportunities to meet new people and connect with others in positive ways.
Connecting with your local, national and international MS communities can be very valuable. Through these, you can learn from others and share your own experiences.
Being a caregiver can be very rewarding. At times, it can also be challenging. If you’re a caregiver, be mindful of signs of depression, anxiety or other mental health conditions. Be active in getting the support and time out you need to care for your mental wellbeing.
If you have people caring for you, ask how they are. Have open conversations together about how each of you is feeling. Support one another.
Tips: How to care for your mental health |
Get professional advice and support. |
Talk to others. |
Have regular mental health checks. |
Practice relaxation. |
Boost your self-management skills. |
MS Canada Resources:
Cognition and MS